Asha Bipolar Clinic (ABC)
Asha Bipolar Clinic (ABC), a unit of Asha Academy of Mood Disorders specialises in the treatment of Mood Disorders and OCD.
The team is headed by Dr M.S. Reddy who has four decades of clinical experience and other members of the team include Dr. Chytanya, Dr. Swetha and Dr Ajay Krishna who share the vision of ABC. Ms. Mansa and Ms. Rachel offer counselling services.
Mood disorders & OCD largely have onset before the age of 25 years, together affecting about 5-10% of the population. Alcohol and other Drug abuse is a common comorbidity (often starting as self-medication) with a cruel fact of 15% ending their lives with suicide
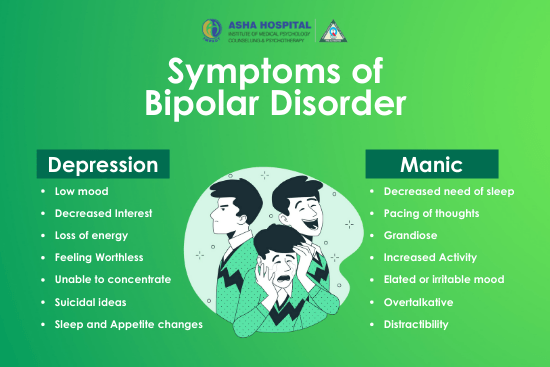
- When a patient has both mania (Pathological “highs”)and depressive episodes it is Bipolar Disorder (BD)
- When there are only depressive episodes it is Depressive Disorder (MDD)
- Premenstrual Mood disturbances are PMDD
- Childhood Mood Dysregulation, Anger outbursts (DMDD)
- Repetitive thoughts (Obsessions), Repetitive Actions (Compulsions) is OCD. The canvas of OCD is very vast including Washing, Checking, Doubts, Symmetry, Blasphemy everything being REPEATED hundreds of times.
The Focus – Mood Disorders and OCD
- Bipolar Disorder (BD)
- Major Depressive Disorder (MDD)
- Disruptive Mood Dysregulation Disorder (DMDD)
- Premenstrual Dysphoric Disorder (PMDD)
- Obsessive Compulsive Disorder (OCD)
Are Depression and OCD becoming more common disorders?
Depression could have been discussed as a common illness after the metric of human life has shifted from Quantity (adding years to life) to Quality (adding life to years) civilisation may not be the large causative factor but probably an inevitable unveiling factor! (Taking an analogy from Cancer – “Cancer became a common illness only when all other killer illnesses, say plague, cholera, TB for ex., have been killed”).
Experiences of Dr M S Reddy as a clinical Psychiatrist over four decades, with focussed attention on mood disorders over two decades; challenges in the management of patients with Mood disorders moments of fulfilling professional satisfaction; helpless feelings of inadequacy, frustrations of “what next and how” not infrequently at therapeutic crossroads on occasions clinical travels with our patients is the journey that led to the conceptualisation of ABC with
Vision: Reinventing “Recovery a Reality” in Mood Disorders
Mission: Evolve Therapeutic Concepts to realise the vision
Four Decades of Clinical Experience, Conviction at Good Prognosis, Unconditional Belief in Science, Will to Doubt with an Open Mind are the four wheels on which ABC moves forward on its chartered path in Mood Disorder management.
- Pharmacotherapy, Counselling and Neuromodulation are the tools
- Good Compliance and Family support are the essentials
Depressive disorder is the dark side of life with slippery bottoms ABC attempts to whisper hope as the mind screams out helplessly Recovery is the Goal and Social Reintegration is the dream.
Meet our Experts: We are here to help you

Dr M S Reddy
Director
Consultant Psychiatrist

Dr Chytanya Deepak P
Director
Consultant Psychiatrist
Dr. Ajay Krishna
Consultant Psychiatrist

Dr Swetha Reddy
Consultant Psychiatrist

Ms Mansa Dantu
Psychologist
FAQ’s
Can I get depressed? Can someone develop depression without psycho-social stress?.
Yes. Depression is biological in origin, has no relation to willpower, can occur without any external reasons. Just like how a person can get an attack of typhoid and recovers with treatment; Depression when itoccurs can be treated.
I am happy why should I be treated? What is the difference between happiness and bipolar Disorder?
In bipolar Disorder, the happiness is short term, unreasonable,irrational and has to be treated.
If I have bipolar disorder, can I return to normalcy?
Symptomatic recovery of the current episode – of any polarity, any degree of severity, any duration, at any age – is the immediate goal. Patient must recover from the current episode (a norm in about 80% patients).
If I have depressive disorder, can I return to normalcy?
In a majority of patients, after recovery from Major Depressive Disorder, life can be as “Normal” as any other average human being! Depressive Disorder – Let us talk, Let us treat. Bring back the smiles…Reintegrate into the society as another well-functioning human!
What kind of treatment can I expect for depression?
Treatment is generally with SSRI antidepressants and counselling. At Asha Bipolar Clinic (ABC) we routinely follow a protocol of SSRI monotherapy, along with counselling which usually is for about 3- 4 sessions at our clinic. A small dose of benzodiazepine is added for relief of anxiety and for better sleep, which is generally stopped after the first few months. Important point to note is that in a majority it takes about 3-4 weeks for the patient to experience significant relief from depression.
- Protocol for Major depressive disorder at ABC is –
- Visit 1 – initial evaluation and diagnosis, starting on antidepressant medication
- Visits 2 to 4 – Counselling sessions, Psychoeducation, Titration of drug dosage (within a period of 7-10 days)
- Visits 5 & 6 – between 4-8 weeks. Remission can be expected around this period
- Visits 7 to 10 – (in those patients who recovered) frequency of visits at 1-2 month intervals.
We down titrate the medication in about 9-12 months based on the levels of improvement This protocol is for majority of patients, but not every patient is treated with same schedule, the plan is individualised. In patients with Psychotic Depression, Chronic depression, Recurrent depression, Bipolar depression etc – Protocols vary with some modifications
Are there any side effects to antidepressants?
SSRI Antidepressants are reasonably safe medicines without any major serious short term and long term adverse events in a majority of patients. But as we all know, no medication can be counted as absolutely safe! Side-effects of SSRIs include GI effects like nausea, vomiting, sexual dysfunction may be seen, they are short term and reversible. Rarely bleeding and hyponatremia maybe seen. Permanent long term side-effects with SSRIs are extremely rare
Do I need life long treatment for bipolar disorder?
The long term course of BD, at least in about a third of patients, is “random and chaotic” and it is nearly impossible to predict the next episode’s onset, polarity, and severity.Recurrence Prevention needs to be based on an individualized long term therapeutic strategy depending on the episodes – frequency, severity, acuteness of onset, suicidality, hospitalization risk, disability….Long term effective prophylaxis (no future episodes) is the desired goal.
Are psychiatry medicines addictive?
Medicines for diabetes and blood pressure are also taken for may years yet they are not seen by the public as addictive! Medicines for mood disorders and OCD are also similar, they are not addictive and the duration of treatment depends on the individual patient.
Is there a difference between wanting things to be clean, orderly and OCD?
Imagine a teenage girl brushing her teeth for 20 minutes, washing hands 33 times, taking 90 minutes for bathing, has to wear this particular coloured dress only on this day of the week, has to check the door lock thrice every time, touch the college bus tyre nine times before getting in, cannot use the college toilet as it is dirty, has to sit cross legged in a specific place in her bedroom before retiring to sleep….an example of a patient with typical OCD symptoms.
Though it has become fashionable to call cleanliness and orderliness as OCD, they are not comparable at all. OCD is a much more serious condition causing lot of morbidity and requiring treatment.
What treatments are available for OCD?
- OCD is one of the major psychiatric disorders, usually starting at the age of 11 – 12, chronic in nature and requires long standing treatment.
- OCD recognised early and treated early has better outcomes.
- Treatment with medication is mandatory and may require high doses of medication at times.
- Promising results is also seen in advanced treatments such as deep TMS and extended ERP/CBT sessions